The Athletic Heart
The benefits of exercise are innumerable, and study after study have demonstrated associations between exercise and a reduction in your risk of heart disease, diabetes, stroke, high blood pressure, and even cancer. This doesn’t event touch on the benefits of exercise from a mental health standpoint, as well as those more difficult to describe aspects – such as motivation, purpose, competition, etc.
Most people know that exercise is good for them, and that they at least should be exercising. But I’m often asked the question (and ponder it myself): can too much exercise be harmful?
The short answer is: possibly. Or, maybe. Actually the short answer is nobody knows for sure. The long answer is more nuanced, and that’s where my own professional interest lies.
Extreme exercise has become somewhat of a focus of the medical community over the past decade or so. The increase in scientific interest has mirrored the significant growth in adult participation in endurance, ultra-endurance, and competitive fitness events (think Ironman and CrossFit). And what medical researchers have found are curious associations between “habitual, vigorous exercise” and negative cardiovascular findings. These include abnormal heart rhythms like atrial fibrillation, evidence of accelerated coronary artery disease, scarring of the heart, and enlargement of the aorta. This has caused many, both in the scientific/medical community and the lay press, to question the benefits of extreme exercise.
But before I get ahead of myself, perhaps we should step back and discuss some of the normal – what we call “physiologic” – changes or adaptations that the heart and cardiovascular system undergo in response to exercise and training. There are many, but I’ll touch on a few important ones here. These adaptations were first described in the 1890’s by the Swedish physician, S. Henschen, when he observed that the hearts of trained Nordic skiers were significantly larger than sedentary individuals. He coined the phrase “athlete’s heart” to describe these changes. While our current understanding is more specific and nuanced, the primary observation is the same – the heart, like any other muscle, adapts to training and in most cases this results in cardiac enlargement, or hypertrophy. Different types of exercise are thought to lead to different cardiac adaptations, a hypothesis which was first proposed by Morganroth in the 1970’s. The Morganroth hypothesis states that aerobic exercise primarily results in eccentric hypertrophy – a balanced increase in both left ventricular (LV) mass as well as LV chamber size – whereas resistance exercise (think weight lifting or wrestling) primarily results in concentric hypertrophy – an increase in LV wall thickness without a change in the chamber size itself. While some have questioned the generalizability of Morganroth’s original hypothesis, the overall concept remains widely accepted. Particularly with endurance training, there is not only enlargement of the LV (the main pumping chamber of the heart), but balanced enlargement of the right ventricle and the atria (top chambers) as well (so called 4-chamber enlargement).
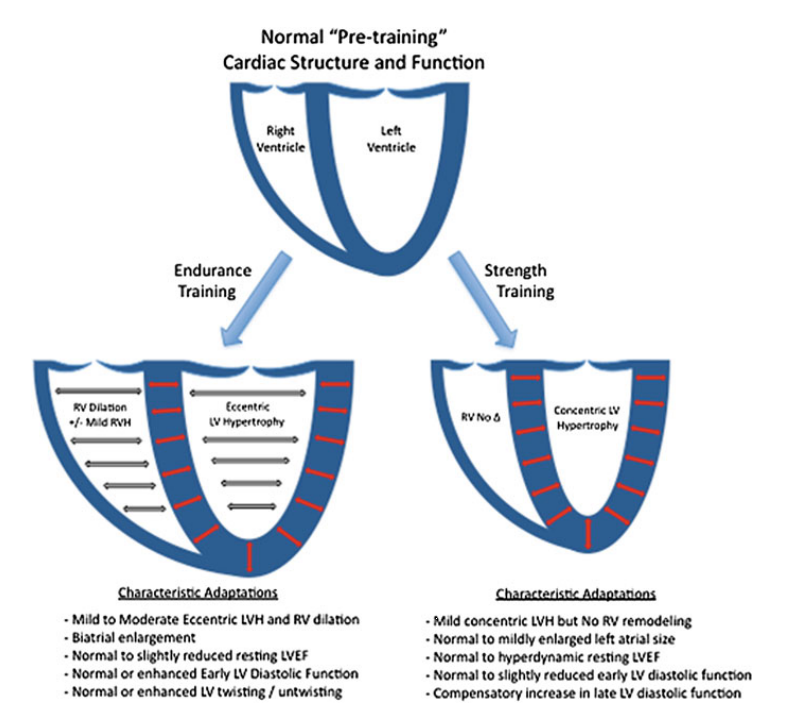
The adaptations described by Morganroth are a framework within which to think about expected changes due to exercise training. There is significant variability in actual changes observed in individual athletes, and much of this is related to the type of sport, intensity/volume of training, race, gender, and other individual factors. Sports with combined endurance and resistance/static components – such as rowing or cycling – tend to result in the most pronounced cardiac adaptations. We have also found that men have more pronounced cardiac enlargement due to training, and African-American athletes generally have increased wall thickness compared to Caucasian athletes.
The driving forces underlying the athlete’s heart are conceptually straight forward. Endurance training stresses the aerobic capacity of the heart and lungs. In order to do aerobic work (as the name implies) the heart and lungs must deliver sufficient oxygen to the muscles. The primary limitation of oxygen delivery in healthy individuals is the ability for the heart to pump an adequate amount of blood (with oxygen carrying red blood cells) to the body – this is called your cardiac output, and is measured in liters of blood per minute. A normal, resting cardiac output is 5-6 liters/min. A highly trained endurance athlete can increase their cardiac output up to 30-40 liters/min! Cardiac output is a simple product of stroke volume – the amount of blood the heart pumps with each beat – and heart rate (CO = SV x HR). Our maximum heart rate is more or less fixed, so the primary way to increase one’s maximum cardiac output is to increase stroke volume, which is why endurance training is considered a “volume challenge” on the heart and leads largely to an increase in cardiac chamber size. Likewise, circulating blood volume expands in response to exercise training to accommodate a higher cardiac output.
There are other characteristic adaptations to exercise. Trained athlete generally have a lower resting heart rate, often 40-60 beats per minute (though occasionally elite athletes will have a resting heart rate in the 30’s). The reduction in resting heart rate reflects two things. The first is that while cardiac dilation and increased stroke volume allows athlete’s the ability to increase their cardiac output with exercise, their cardiac output at rest is relatively unchanged. To achieve the same cardiac output at rest (remember CO = HR x SV), their resting heart rate is reduced. The second reason for resting heart rate reduction is a shift in activity of the autonomic nervous system. This is the part of the nervous system that unconsciously regulates our body systems, including things like heart rate and blood pressure. Exercise leads to an increase in the parasympathetic nervous system (or vagal tone), and a decrease in resting activity of the sympathetic nervous system (the so called “fight or flight” response that we learn in high school biology).
Because of chamber dilation, the contractile function of the athletic heart may appear mildly reduced at rest. Cardiologists commonly reference the “ejection fraction” – or percentage of the left ventricular blood volume that is ejected with each heart beat – as a measurement of contractile function. Highly trained endurance athletes may have resting ejection fractions between 45-50% (normal >52%). You can imagine that a physician or cardiologist who is not accustomed to evaluating trained athletes may be quite concerned when they come across an athlete with a heart that appears weak and dilated, and think that there must be a disease of the heart muscle. In fact, one of the common questions that a Sports Cardiologist is asked to answer is whether findings in an athlete represent expected changes due to training, or represent an abnormality that should be further evaluated. Only by understanding the expected changes, accounting for the athlete’s age, gender, race, and specific sport/training regimen, can we then answer this important question.
While there are numerous other adaptations to exercise (some of which I may delve into in the future), these are the basic, physiologic adaptations that occur from a cardiovascular standpoint, and those that define the namesake of this blog, The Athletic Heart.
In Part 2 of this series on “Exercise and the Heart”, I’ll discuss extreme exercise, its impact on the heart, and the frequently asked question: can too much exercise be harmful?

1 Reply to “Exercise and the Heart: Part One”
Comments are closed.